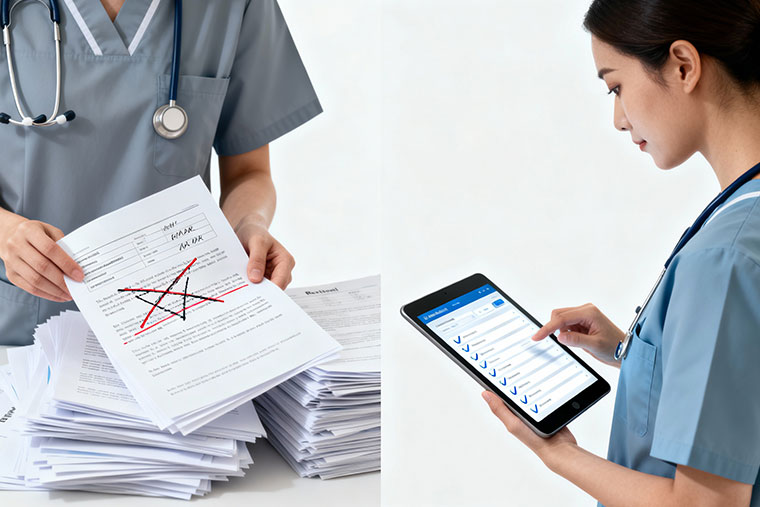
In healthcare, an efficient referral management system is essential for ensuring patients receive the care they need promptly. A referral system that seamlessly connects providers and patients ensures that no opportunity is missed, especially when a patient’s condition requires a specialist’s attention. However, traditional referral management systems are often plagued with inefficiencies, especially when it comes to processing referrals after hours.
The integration of Voice AI and automated referral platforms has changed the way referrals are managed, creating a streamlined process that spans from patient consultation to follow-up care. This step-by-step journey will walk you through the entire referral management cycle, from the initial consultation to the final follow-up, showcasing how automation and integration drive greater efficiency and improved patient care.
Step 1: Patient Consultation – The Starting Point

The journey of referral management begins with patient consultation, which is often the first point of contact between a healthcare provider and a patient. This stage is critical, as it sets out the foundation for the referral process.
Key Activities:
- Assessing the Patient’s Condition: During the consultation, healthcare providers listen to the patient’s symptoms, medical history, and any concerns. The provider evaluates whether the patient's condition requires a referral to a specialist or diagnostic center.
- Decision to Refer: The healthcare provider may decide that the patient needs additional expertise or diagnostic tests beyond their own capabilities, prompting a referral to a relevant specialist or medical facility.
- Information Gathering: Data is collected, including patient demographics, previous medical history, current medications, and allergies. This information is critical for ensuring that the referral is appropriate and accurate.
Benefits:
- Accuracy in Referral: By gathering detailed patient data, healthcare providers can make well-informed decisions about referrals, reducing the likelihood of unnecessary or incorrect referrals.
- Improved Patient Satisfaction: When the need for a referral is clear, patients can feel confident that they are being directed to the right care provider without unnecessary delays.
Explore how EMR/EHR systems enhance consultation data accuracy and streamline the patient intake process here.
Step 2: Referral Creation in EMR/EHR – Streamlining the Process

Once a referral is deemed necessary, the next step is the creation of the referral within the EMR/EHR (Electronic Medical Record / Electronic Health Record) system. This step eliminates paper-based records and facilitates the digital transfer of referral information.
Key Activities:
- Automated Data Population: When creating a referral, patient data such as diagnosis, medical history, and demographics are automatically pulled from the existing medical records in the EMR/EHR system. This reduces the need for manual entry, minimizing the risk of data errors.
- Referral Details: The healthcare provider enters the key information for the referral, including:
- Specialist’s Name: The provider to whom the referral is being made.
- Reason for Referral: A detailed explanation of the patient’s condition and the required treatment or tests.
- Urgency: Whether the referral is urgent or routine, helping to prioritize the referral appropriately.
- Electronic Document Generation: The system can automatically generate a referral document, which includes the patient’s relevant information and a brief summary of the medical situation. This document is then sent to the receiving provider or facility.
Benefits:
- Minimized Errors: Automatic data population reduces human errors, ensuring accurate and complete referral details.
- Faster Referral Process: With digital systems, referrals are created more quickly than with traditional manual methods, reducing wait times for patients.
Learn how EMR/EHR integration simplifies referral creation and supports better patient outcomes here.
Step 3: Referral Submission to Hospital/Diagnostic Center – Seamless Transition

After the referral is created, the next step is to submit the referral to the appropriate hospital or diagnostic center. This is a critical part of the referral management process, as it ensures the right specialists are notified immediately.
Key Activities:
- Electronic Submission: Once the referral is created in the EMR/EHR system, it is electronically submitted to the hospital, clinic, or diagnostic center. This eliminates the need for paper-based referrals and speeds up the process, ensuring no time is wasted.
- Documentation Sharing: Along with the referral, additional documentation, such as lab results, medical imaging, and the patient’s medical history, is shared with the receiving healthcare provider to give them a full understanding of the patient’s needs.
- Real-Time Acknowledgment: The receiving provider acknowledges the referral, ensuring that both the referring physician and the specialist are aligned on the next steps.
Benefits:
- Faster Action: With electronic submission, the specialist or diagnostic center can immediately review the referral and plan accordingly, preventing delays in the patient’s care.
- Reduced Paperwork: Eliminating paper-based referrals saves time, reduces administrative burden, and minimizes the risk of lost or misplaced paperwork.
Find out how automated referral systems streamline the submission process and ensure faster care delivery here.
Step 4: Triage – Prioritizing the Referral
Once the referral reaches the hospital or diagnostic center, it goes through the triage process. Triage is the process of determining the urgency and importance of a referral, ensuring that patients receive timely attention.
Key Activities:
- AI-Powered Triage: Many referral systems now integrate artificial intelligence (AI) to evaluate the urgency of a referral based on predefined criteria (e.g., medical history, symptoms, or diagnosis). This helps prioritize critical cases that need immediate attention.
- Manual Review: In some cases, triage nurses or administrative staff may manually review the referral to assess its urgency, especially in complex cases that require further evaluation.
- Urgency Categorization: Referrals are categorized into different levels of urgency (e.g., emergency, urgent, routine), which helps the healthcare provider prioritize their workload.
Benefits:
- Improved Care Delivery: Urgent referrals are processed first, ensuring that critical cases are handled without delay.
- Resource Optimization: Triage helps optimize the use of hospital resources by ensuring that staff are not overwhelmed with non-urgent cases when more critical patients require attention.
See how AI-driven triage improves patient care by prioritizing urgent cases here.
Step 5: Scheduling – Setting Up Appointments

After the referral has been triaged, the next step is scheduling the appointment for the patient. This step ensures that the patient is seen by the right specialist at the right time.
Key Activities:
- Automated Appointment Booking: Integrated referral platforms automatically book an appointment with the specialist or diagnostic center, considering both the patient's and provider's availability.
- Appointment Notifications: Once the appointment is scheduled, both the patient and the healthcare provider receive confirmation notifications, reducing the risk of missed appointments and improving communication.
- Multiple Appointment Options: Some systems offer the ability for patients to select available time slots, providing flexibility for both parties.
Benefits:
- Efficient Use of Time: Automated scheduling reduces the time spent coordinating appointments, improving overall clinic efficiency.
- Improved Patient Engagement: Automated notifications and reminders help keep patients informed, reducing no-shows and enhancing patient satisfaction.
Explore how automated scheduling systems improve patient experience and reduce no-shows here.
Step 6: Care Coordination – Ensuring Comprehensive Treatment

Effective care coordination ensures that patients receive comprehensive care across all touchpoints—whether it's the initial consultation, specialist appointment, or follow-up care.
Key Activities:
- Inter-Provider Communication: Care coordination platforms enable seamless communication between the referring physician, specialists, and diagnostic centers, ensuring that all providers are aligned on the patient’s treatment plan.
- Follow-Up Planning: The referring doctor may create a follow-up plan for the patient, including additional tests or a future check-up after treatment.
- Patient Education: Patients are informed about their treatment plan, ensuring they understand the next steps in their care journey.
Benefits:
- Comprehensive Care: By coordinating care across multiple providers, patients receive a holistic and streamlined treatment plan, ensuring better health outcomes.
- Fewer Care Gaps: Improved communication reduces the risk of missed treatments or conflicting treatment plans.
Learn how care coordination ensures continuity of care and improves patient outcomes here.
Step 7: Follow-Up & Completion – Closing the Referral Loop

The final step in the referral management journey is the follow-up and completion of the referral process. This step ensures that the patient receives proper follow-up care and that all parties are updated on the treatment progress.
Key Activities:
- Post-Treatment Follow-Up: A follow-up appointment may be scheduled to check the patient's progress or ensure that the treatment plan is working.
- Referral Completion: Once the patient has received care and any follow-up actions are completed, the referral is closed in the system. The referring physician is updated with a report on the specialist’s findings and treatment outcomes.
- EHR Integration: All new data and treatment outcomes are integrated back into the patient’s EMR/EHR, ensuring that their medical record is up-to-date and accessible for future care.
Benefits:
- Complete Treatment: Ensures the patient receives all the necessary care from initial consultation to follow-up.
- Better Patient Record Keeping: The completion of the referral closes the loop and ensures that the patient’s records are comprehensive and accurate.
Read more about how follow-up care enhances patient satisfaction and treatment success here.
Conclusion: Ensuring a Smooth Referral Journey
Referral management is a complex, multi-step process that requires efficiency, accuracy, and communication. By integrating EMR/EHR systems, automated referral platforms, and care coordination tools, healthcare providers can streamline each stage of the referral journey from consultation to follow-up ensuring that patients receive timely and comprehensive care.
The use of automation and AI-driven solutions in referral management not only reduces administrative burdens but also improves patient outcomes by eliminating bottlenecks and inefficiencies. As healthcare systems continue to evolve, embracing automated referral solutions will become even more essential for ensuring that no patient is left behind.