1 | Introduction — The “ADT-at-2 a.m.” Problem
Picture a nurse on the night shift: the resident arrives, but the HL7 ADT (admit-discharge-transfer) message never does. Allergies are unknown, the med list is lost in transit, and what should be a calm hand-off turns into frantic detective work. Scenarios like this play out nightly because post-acute organizations still rely on brittle point-to-point interfaces built for a single hospital, not for a web of referral partners.
Meanwhile, the Trusted Exchange Framework and Common Agreement (TEFCA) is accelerating the push toward real-time, nationwide data exchange. QHINs—the clearinghouses that make TEFCA work—are already onboarding long-term-care and post-acute participants, and policy analysts say 2025 is the year “interoperability moves from paperwork to production.”
Bottom line: data chaos isn’t destiny—it’s an operations problem. Modern interface engines, FHIR “façade” services, and disciplined governance can turn those 2 a.m. mysteries into lights-out, automated interoperability.
2 | Why HL7 Feels Harder in Post-Acute Settings
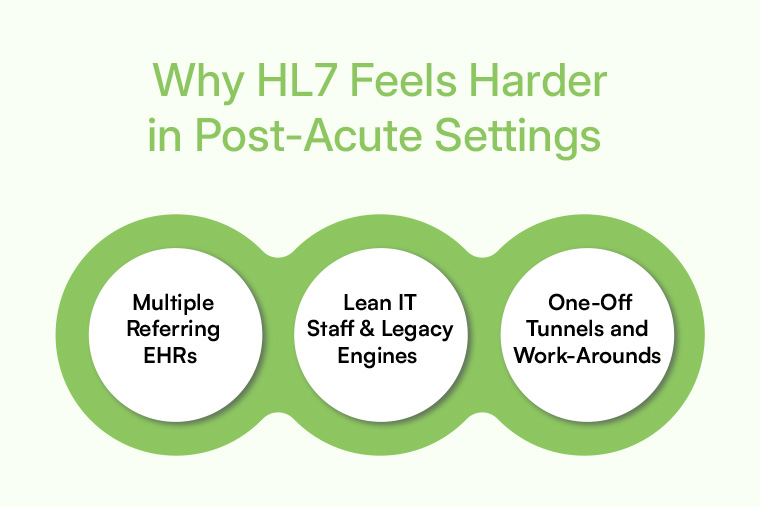
Multiple Referring EHRs
Hospitals often run Epic or Cerner, but post-acute providers may also receive referrals from MEDITECH, PointClickCare, or regional HIE portals. Each system speaks its own dialect of HL7 v2.x or partial FHIR bundles, forcing admissions teams to juggle a spaghetti bowl of mappings.
Lean IT Staff & Legacy Engines
A 2024 ONC brief found that only 17 percent of hospitals can “routinely” send or receive data with LTPAC facilities—largely because their downstream partners run decade-old interface engines and have a single analyst covering everything from billing reports to printer jams.
One-Off Tunnels and Work-Arounds
Quick-fix VPNs, SFTP drops, and “remote printers” spring up every time a new partner connects. Each workaround solves a short-term need but leaves behind tech debt that will break with the next Windows patch.
Add chronic staffing shortages, and it’s no surprise clinical teams treat the integration stack as unstable black-box plumbing—better left untouched.
3 | Decoding the Alphabet Soup: HL7 v2.x vs. FHIR R4
HL7 v2.x has moved healthcare messages since the 1990s—compact, pipe-delimited, and optimized for ADT and lab orders. FHIR R4, by contrast, delivers web-style JSON resources, granular scopes, and OAuth-powered security.
Adoption is snowballing:
- A global 2025 survey of 82 HL7 affiliates shows 78 % of jurisdictions now have regulations accelerating FHIR adoption, up from 52 % two years ago.
- Analyst forecasts expect 90 % of health systems to expose at least one FHIR API by year-end 2025.
Where HL7 still rules
- Admit, discharge, and transfer notifications
- Lab and radiology results
- Pharmacy dispense messages
Where FHIR shines
- Dynamic resources like problem lists, care plans, and med reconciliations
- SMART-on-FHIR apps that embed directly in a PointClickCare or Epic frame
- Bulk-data exports for quality reporting and population analytics
Most post-acute providers must bridge both standards—yes to the trusty HL7 feed, yes to the modern FHIR API, and yes to whatever the next partner brings. The only realistic path is architectural: one conversion layer that can translate at wire speed.
4 | Five Proven Tactics to Tame Data Complexity

4.1 Centralize Feeds in a Cloud Interface Engine
Moving from many point-to-point feeds to a managed, cloud-hosted engine removes server maintenance, adds 99.9 % uptime SLAs, and auto-scales during flu-season surges. Integration-engine vendors such as Rhapsody and Corepoint top the 2025 Best in KLAS rankings precisely because providers say cloud delivery “just works.”
Explore more: Cabot Healthcare Integration Services
4.2 Wrap Legacy HL7 with a FHIR Façade
A FHIR façade ingests incoming HL7, applies vocab-mapping rules, and exposes polished FHIR APIs to mobile apps, AI triage tools, or external partners. Upstream hospitals continue to send the same messages; downstream innovators enjoy an elegant API surface.
Explore more: Cabot Interoperability Solutions
4.3 Automate Vocabulary Mapping
Misaligned codes tank authorizations and muddy analytics. Automated crosswalks among LOINC, SNOMED, and NUBC keep med lists tidy and claims squeaky-clean. Industry blogs still rank vocabulary mismatches as the top hidden cost of HL7 projects.
4.4 Enforce Upstream Data-Quality Rules
Instead of fixing bad data downstream, validate at the gate—missing MRNs, payer IDs outside your allow-list, or unknown allergies generate immediate alerts. Clinicians receive complete meds lists, and billing submits first-pass clean claims.
4.5 Monitor Interfaces in Real Time
Dashboards that track message volume, latency, and error spikes convert “mystery downtime” into proactive remediation. Most cloud engines push alerts to Microsoft Teams, email, or SMS, letting one analyst support dozens of facilities without the usual pager days.
5 | TEFCA & 2025 Interoperability Deadlines—What Post-Acute Execs Need to Know
- Participation becomes the new referral currency. Large hospital groups already ask whether SNF partners can connect through a QHIN node, and payer contracts increasingly reward “TEFCA-ready” status.
- FHIR bulk files are coming fast. Population-health programs and quality-reporting pilots are shifting from HL7 CCDs to FHIR NDJSON exports—providers need at least one receiving endpoint.
- Security attestations ride the connection. Cloud engines that are HITRUST or SOC-2 verified shorten onboarding when a QHIN demands proof.
Ignoring TEFCA won’t draw federal fines today, but it can quietly lock a facility out of high-margin referral networks tomorrow.
6 | ROI Without a Spreadsheet: Three Benefits That Sell Themselves
- Nurse Satisfaction
When meds and allergy lists arrive intact, clinicians spend evenings with residents, not the fax machine.
- Referral Loyalty
Discharge planners trust facilities that reply, “Yes, we see your feed live,” rather than “Fax it again and we’ll get back to you.”
- IT Agility
A cloud engine lets one analyst spin up a new feed in days—an edge when a payer rolls out a new quality-bonus program or a hospital joins TEFCA.
Real-world inspiration: How a Custom Digital Solution Transformed PAC Coordination
7 | Action Checklist for a Low-Risk Rollout

- Audit Every Connection
List HL7 feeds, VPN tunnels, and hand-keyed imports. Visibility precedes control.
- Prioritize High-Pain Workflows
Start with ADT and meds reconciliation—the two most disruptive gaps.
- Pick an Enthusiastic Pilot Partner
A hospital liaison eager for real-time status updates accelerates troubleshooting.
- Define Success Metrics
Message latency < 60 seconds, manual re-entry hours reduced 75 %, first-pass clean claims > 95 %.
- Review the Dashboard Weekly
A five-minute huddle keeps momentum, surfaces early wins, and builds trust with clinical staff.
8 | Conclusion — From Data Chaos to Seamless Continuity of Care
The next time a resident rolls in at 2 a.m., every nurse should have allergies, meds, and care plans at their fingertips. By centralizing feeds, wrapping legacy HL7 in a FHIR façade, and enforcing data-quality rules upstream, post-acute organizations turn tangled interfaces into strategic infrastructure. Regulatory pressure is only going to tighten, but early movers already enjoy smoother admissions, happier clinicians, and stronger referral pipelines.
Interoperability isn’t a moon-shot; it’s a disciplined series of fixes that compound. Start with one feed, one partner, one dashboard—and watch the dominoes fall.
Experience Cabot’s integration accelerator and discover how quickly you can simplify HL7 & FHIR interfaces.