1. Introduction: The Challenge of Readmissions in Skilled Nursing Facilities
Readmissions to hospitals from Skilled Nursing Facilities (SNFs) are a significant concern for both healthcare providers and patients. A high readmission rate not only affects patient outcomes but also impacts the facility’s financial health. The Centers for Medicare & Medicaid Services (CMS) impose penalties on SNFs with high readmission rates, urging them to improve discharge planning processes to ensure better patient transitions.
One of the most effective ways to mitigate readmission risks is through a thorough and well-executed discharge planning process. This ensures patients leave with all the necessary instructions, follow-up care plans, and support systems in place.
In this blog, we’ll explore how smart discharge checklists can enhance the discharge process, reducing the chances of unnecessary readmissions and improving patient outcomes.
2. The Importance of Discharge Planning in Reducing Readmission Risks
Discharge planning is a critical part of care in Skilled Nursing Facilities, ensuring that patients leave with the right resources, support, and follow-up care. Without a comprehensive plan, patients are at a higher risk for complications that could lead to a readmission, including:
- Medication errors: Patients may not fully understand how or when to take their medications.
- Missed follow-up care: Patients may forget to schedule follow-up appointments or fail to attend them.
- Lack of caregiver support: Without proper assistance, patients might struggle to manage their health at home.
Studies show that when discharge planning is executed properly, it reduces readmission risks and contributes to better long-term health outcomes. This is where a smart discharge checklist can help.
3. How Smart Discharge Checklists Enhance Patient Outcomes
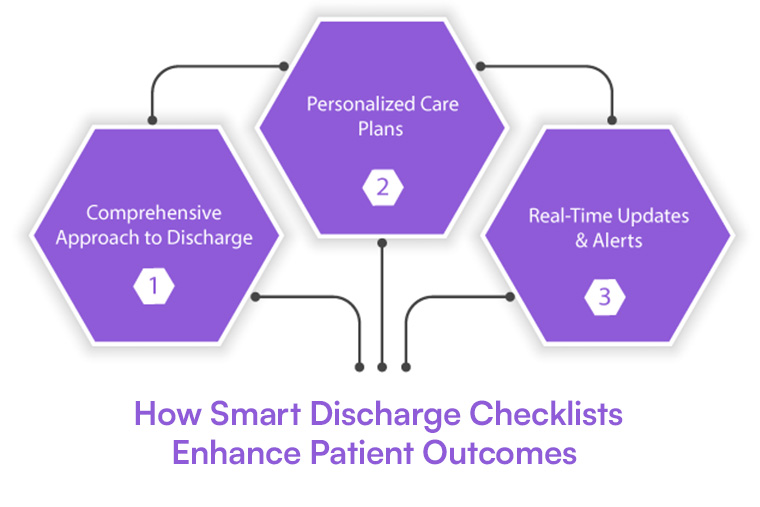
Smart discharge checklists are an essential tool in reducing readmission risks. These checklists utilize technology to ensure that every step of the discharge process is completed efficiently and accurately. Here are several ways smart checklists improve patient outcomes:
3.1 A Comprehensive Approach to Discharge
A smart discharge checklist ensures that the discharge process includes all necessary elements to prepare the patient for a successful transition. These checklists include sections on:
- Medication reconciliation: Confirming the medications the patient should take, potential side effects, and instructions on how to manage them.
- Care instructions: Specific instructions about the patient’s condition, recovery process, and any lifestyle adjustments.
- Follow-up appointments: Ensuring that necessary follow-up appointments are scheduled and that patients understand their importance.
- Caregiver education: Ensuring caregivers are equipped with the knowledge needed to support the patient’s recovery at home.
By breaking down the discharge process into clear steps, SNFs ensure that nothing is missed, and patients leave with all the necessary tools for success.
3.2 Personalized Care Plans
Smart discharge checklists enable personalized care for each patient. By integrating data from the patient’s Electronic Health Record (EHR), SNFs can tailor the checklist to the individual’s health condition, needs, and post-discharge plan. This ensures that the patient receives instructions specific to their condition, minimizing the risk of complications after discharge.
3.3 Real-Time Updates and Alerts
Smart discharge checklists can trigger alerts and reminders for SNF staff if any steps are incomplete, reducing the risk of errors. For example, if a medication review hasn’t been completed or a follow-up appointment hasn't been scheduled, the system will automatically remind staff to complete those tasks.
4. Smart Discharge Checklist: A Practical Tool for SNFs

The following Smart Discharge Checklist can be used by Skilled Nursing Facilities to ensure that all necessary steps are covered before a patient is discharged. This checklist can be integrated into digital systems or used manually as a guide.
Smart Discharge Checklist
1. Patient Identification
- Verify patient’s name, date of birth, and medical record number.
- Review patient's medical history and current condition.
2. Medication Reconciliation
- Confirm all medications prescribed at discharge.
- Ensure patient and caregiver understand when and how to take each medication.
- Check for potential drug interactions or changes to the patient’s medication.
- Provide written medication instructions for patient/caregiver.
3. Follow-Up Care
- Schedule follow-up appointments with primary care providers or specialists.
- Educate patient and caregiver about the importance of attending appointments.
- Share contact information and directions for follow-up appointments.
4. Caregiver Education
- Educate caregivers on their responsibilities in supporting the patient’s recovery.
- Review any home care needs (e.g., physical therapy, nursing visits).
- Provide caregiver instructions (how to manage medications, monitor for complications).
5. Patient Education
- Provide discharge instructions in simple, easy-to-understand language.
- Include details on dietary restrictions, activity limitations, and warning signs to look out for.
- Educate when to seek medical help if symptoms worsen or if emergency care is needed.
6. Post-Discharge Resources
- Share details about community resources, such as support groups or home health services.
- Confirm the patient has access to transportation for follow-up appointments.
- Provide emergency contact numbers .
7. Final Confirmation
- Verify that patient and caregiver understand all discharge instructions.
- Answer any remaining questions from the patient or caregiver.
- Confirm that the checklist is completed before discharge.
5. The Role of Technology in Implementing Effective Discharge Checklists
Leveraging technology in discharge planning can significantly improve efficiency, accuracy, and collaboration. By incorporating different levels of technological solutions, Skilled Nursing Facilities (SNFs) can ensure that the discharge process is streamlined and that patients receive the right care during their transition. Let's explore the basic, advanced, and AI-integrated levels of technology and their unique advantages:
5.1 Basic: Digital Checklists for Enhanced Coordination
At the basic level, moving from traditional paper-based checklists to digital checklists is an essential first step. Digital checklists allow for better organization, reduce paperwork errors, and provide real-time access to discharge information for care teams.
Advantages:
- Real-time updates: Care team members, such as doctors, nurses, and discharge coordinators, can update and access the checklist instantly, ensuring that every task is completed without delays.
- Improved coordination: Nurses can check off completed tasks, flagging anything that requires further attention, and communicate any updates directly with the care team.
- Reduced errors: Digital checklists eliminate the risk of missing steps or incomplete information that is often common with manual paper records.
At Cabot Technology Solutions, we specialize in developing cloud-based platforms that facilitate digital checklists, allowing for seamless care team coordination and timely updates.
5.2 Advanced: EHR Integration for Accuracy and Efficiency
At the advanced level, integrating the smart discharge checklist with a facility's Electronic Health Records (EHR) enhances the process further by ensuring that all patient data used in the checklist is accurate and up-to-date. This integration provides a more seamless experience, reducing the chances of human error and ensuring comprehensive care planning.
Advantages:
- Accurate data transfer: Patient medical history, medications, and follow-up needs are pulled directly from the EHR, ensuring that no information is missed or duplicated.
- Streamlined workflows: Care team members can work within a single system to access patient data and discharge tasks without switching between different platforms.
- Improved decision-making: Having access to real-time EHR information allows healthcare providers to make well-informed decisions about follow-up care and post-discharge support.
This integration leads to more efficient discharge planning and reduces the chance of critical information being overlooked during the transition process.
5.3 AI-Integrated: Predictive Analytics for Risk Assessment
At the AI-integrated level, the discharge checklist can be enhanced with predictive analytics that analyze patient data and predict which individuals are at higher risk for readmission. By incorporating artificial intelligence (AI), SNFs can proactively address the needs of high-risk patients, ensuring that they receive additional support and care after discharge.
Advantages:
- Risk prediction: AI analyzes historical patient data, health conditions, and social factors to predict which patients are more likely to be readmitted, enabling the care team to take preventive action.
- Personalized follow-up care: High-risk patients can be flagged for additional interventions, such as more frequent follow-ups or home healthcare services, improving their chances of a successful recovery.
- Data-driven decision-making: Predictive analytics can guide care teams on the level of post-discharge care needed, ensuring that no patient falls through the cracks.
Using AI not only improves the accuracy of discharge planning but also enhances patient outcomes by providing targeted interventions where they are most needed.
By incorporating basic, advanced, and AI-integrated technology into the discharge planning process, Skilled Nursing Facilities can greatly improve the quality of care and reduce readmission risks. Whether starting with digital checklists or advancing to AI-powered analytics, each level brings added value to ensuring a smooth transition for patients.
At Cabot Technology Solutions, we specialize in helping SNFs integrate these technological solutions to streamline discharge planning and improve patient outcomes. Contact us today to learn more about how we can support your facility’s goals.
6. Best Practices for Building and Using Smart Discharge Checklists
The successful use of smart discharge checklists requires more than just the right technology. Skilled Nursing Facilities should follow best practices to ensure the system’s success:
6.1 Training Healthcare Teams
Staff members need to be thoroughly trained on how to use the smart discharge checklist system. This includes understanding how to update patient records, interpret alerts, and communicate with the rest of the care team.
6.2 Engaging Patients and Caregivers
Patients and caregivers should be active participants in the discharge process. They should be given the opportunity to ask questions, confirm their understanding of discharge instructions, and ensure that they are fully prepared for the transition home.
6.3 Continuous Monitoring and Feedback
Facilities should track the effectiveness of their discharge checklists by monitoring outcomes, such as readmission rates and patient satisfaction scores. Continuous feedback should be gathered to make improvements in the discharge process.
7. Conclusion: How Cabot Solutions Can Help Improve Patient Care and Reduce Readmission Risks

Reducing readmission risks in Skilled Nursing Facilities is a complex task that requires comprehensive discharge planning. By incorporating smart discharge checklists, SNFs can ensure that every patient leaves with the necessary tools for a successful recovery. These checklists ensure that critical steps—like medication reconciliation, follow-up appointments, and caregiver education—are not missed.
At Cabot Technology Solutions, we specialize in integrating advanced technology solutions that support effective discharge planning. Our EHR integration, telehealth services, and cloud-based systems can help SNFs implement smart discharge checklists that improve patient care and reduce readmission rates.
Contact Cabot Technology Solutions today to learn how we can help optimize your discharge planning process and improve patient outcomes.

