Introduction: The Unseen Crisis in Hospital Referrals
Every day, hospitals across the U.S. face a hidden bottleneck: discharging patients to post-acute care (PAC). These include skilled nursing facilities, inpatient rehab, long-term care, or even home health. Yet, the transition from hospital to PAC is often delayed—not because of medical issues, but due to outdated referral processes.
These delays increase length of stay, reduce bed availability, hurt patient satisfaction, and cost hospitals money. At a time when hospital margins are tighter than ever, an inefficient referral process can ripple across the entire health system.
That's where AI-powered referral management steps in—automating decisions, accelerating placements, and delivering real results.
What Is AI‑Powered Referral Management?
AI-powered referral management platforms use artificial intelligence, predictive analytics, and machine learning to automate:
- Matching patients with PAC providers involves analyzing clinical data, insurance coverage, proximity, and facility ratings to suggest the most appropriate care setting for the patient's recovery needs. AI tools use historical outcome data to improve the quality of matches over time.
Sending referrals with complete documentation is streamlined by integrating directly with the hospital's EHR. This allows AI systems to auto-populate forms with accurate, up-to-date patient information, including diagnoses, lab results, medications, and insurance details, minimizing errors and omissions.
Communicating in real-time enables care coordinators and PAC providers to interact on a shared digital platform. Providers can accept or reject referrals, request more information, and coordinate next steps without relying on faxes or phone calls.
Tracking progress and outcomes offers full visibility into every step of the referral journey. Coordinators can see which providers have received, opened, and acted on referrals, along with timestamps, while also tracking patient outcomes post-discharge to evaluate referral effectiveness.
Predicting risks, delays, or denials before they occur is possible through machine learning models trained on referral history. The system can flag high-risk cases early, suggest alternate PACs, and guide staff through resolution paths—reducing delays and improving continuity of care.
Core Components:
- Smart Matching: AI evaluates patient needs (diagnosis, therapy requirements, mobility status, insurance coverage, etc.) and compares them against real-time PAC data to match the best facilities.
- Automated Documentation: Pulls data directly from the hospital’s EHR to eliminate redundant entry and ensure accurate, complete referral packets.
- Live Communication: Enables PAC facilities to accept, reject, or request clarification digitally.
- Predictive Alerts: Flags high-risk patients or likelihood of referral delays using historical and real-time patterns.
Real-World Scenario: Before vs. After AI
Before AI
- A 78-year-old patient is cleared for discharge after hip surgery.
- Referral is faxed to 4 SNFs. Only 2 respond in 6 hours.
- SNFs request additional info not included initially.
- One facility is full, the other denies due to insurance mismatch.
- Case manager spends hours in follow-ups. Patient waits 26 hours before transfer.
After AI Implementation
- Referral is triggered automatically when discharge order is placed.
- AI pre-fills all clinical and insurance data.
- Top 3 suitable SNFs (in-network, beds available, rated for ortho rehab) identified.
- Referral sent instantly with digital documents.
- First facility accepts within 20 minutes; transport arranged within the hour.
Outcome: Discharge in 3.5 hours instead of 26. One hospital bed freed up. Better continuity of care.
Step-by-Step Breakdown: How AI Improves the Referral Process

- Trigger from Discharge Workflow
AI listens for discharge orders in EHR. No manual initiation needed.
- Clinical Data Pull & Form Auto-Fill
Data like ICD-10 codes, medications, vitals, and insurance details are pulled and formatted per provider needs.
- PAC Matching Engine
Machine learning ranks PAC options based on criteria like patient outcomes, availability, past referral history, and geographic proximity.
- Digital Referral Dispatch
Instead of fax, referrals are sent electronically via secure channels. PAC facilities receive complete info instantly.
- Real-Time Tracking
Referral coordinators can see which providers have opened, responded, or not yet acted.
- Alerts & Escalation
If a referral isn’t accepted within a timeframe, the system flags it, suggests alternatives, or escalates to a manager.
- Analytics & Learning
The platform learns from outcomes to improve future matches—e.g., SNF A responds faster to ortho rehab patients than SNF B.
The Tangible Benefits
Other benefits:
- Reduced bed blocking
- Better PAC placement quality
- Improved HCAHPS scores
- Lower nurse coordinator burnout
Pain points tackled
- Reduced Length of Stay: Each extra day costs $2,000–$4,000 depending on region.
- Improved care continuity: Fragmented transitions mean worse outcomes.
- Minimized network leakage: Referred outside the system = lost revenue.
- Strengthened provider partnerships: Lack of feedback loops with PAC facilities creates blind spots.
ROI: Cost vs. Value Breakdown
For a 250-bed hospital:
- $250,000–$400,000/year saved through reduced LOS and staffing time
- 20% drop in readmissions from better PAC alignment
- Stronger PAC network integrity and lower leakage
Break-even on platform investment in under 6 months for mid-sized systems.
"We reduced our average discharge delay by 16 hours within the first month. The impact on throughput and team morale was immediate." — CMIO, Regional Health System
Technical Highlights for Implementation Teams
- Security: End-to-end encryption, HIPAA-compliant, SOC 2 Type II
- APIs & Integration: Supports FHIR, HL7, and EHR connectors for Epic, Cerner, Meditech
- User Roles: Admin, coordinator, PAC provider, executive reporting access
- Deployment Time: 4–6 weeks with phased go-live
- Training & Support: Typically 3–5 sessions; low learning curve
Risks of Staying Manual

Hospitals that avoid modernization face:
- Higher inpatient costs due to discharge delays Delays in referrals directly translate to longer patient stays in costly acute care settings. For every additional day a patient occupies a bed post-clearance, the hospital incurs $2,000–$4,000 in extra costs, without additional reimbursement. This not only affects margins but also blocks bed access for incoming admissions.
- Staff frustration and burnout in care coordination Manual referral processes overwhelm care coordinators, discharge planners, and nurse managers with repetitive paperwork, follow-up calls, and constant troubleshooting. The inefficiency contributes to staff burnout, low morale, and turnover—especially during peak discharge times.
- Poor discharge experience leading to lower HCAHPS Patients and families experience stress and dissatisfaction when discharges are delayed or poorly communicated. These negative experiences are reflected in Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, which impact hospital ratings and Medicare reimbursements.
- Increased readmission rates due to mismatched PAC placement Without data-driven matching, patients may be referred to facilities that are not best equipped to handle their recovery needs. This increases the likelihood of complications, ER returns, and readmissions—penalizing hospitals under value-based purchasing models.
- Lost patients to outside networks with digital tools Patients referred to external networks or facilities with better coordination platforms may never return to the original health system for future care, resulting in leakage and lost lifetime value. Hospitals without modern tools risk losing their competitive edge and patient loyalty.
In short, relying on fax and phone calls is costing time, money, and care quality.
Getting Started: Key Steps to Adoption
- Assess Your Current Workflow
Begin by auditing your current referral management process. Identify average referral volume per month, typical turnaround times, bottlenecks, and leakage points where patients exit the network. Understand which departments experience the most delays and why.
- Engage PAC Providers
Contact your most frequently used PAC facilities and assess their readiness to receive referrals digitally. Help onboard them to the platform or encourage them to adopt compatible technology. Strong collaboration at this stage sets the foundation for smoother coordination.
- Pilot Program
Choose a department with high patient turnover—like orthopedics, cardiology, or neurology—and implement the AI-powered referral tool in a limited, controlled environment. This allows your team to test, refine, and build internal champions for broader rollout.
- Train Discharge Teams
Conduct scenario-based training with your discharge planners and case managers. Walk them through real patient examples using the new tool, and clarify how their daily tasks will change. Include checklists, video tutorials, and a feedback loop for ongoing support.
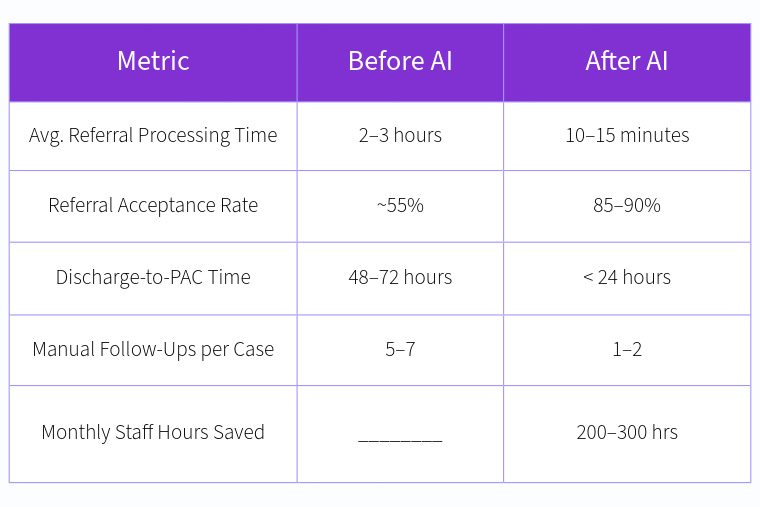
- Measure Results
Track key metrics such as referral processing time, PAC acceptance rate, average length of stay, and staff hours saved. Collect both qualitative and quantitative feedback to refine workflows and build the business case for full-scale implementation.
Final Thoughts
AI-powered referral management transforms one of healthcare’s most overlooked friction points: transitioning patients from acute hospital care to the most suitable post-acute care (PAC) setting. These referral transitions are critical not only for bed management but also for patient recovery outcomes and hospital operational efficiency. With AI, the process becomes faster, more accurate, and far less dependent on manual intervention.
- Free up beds without cutting corners: By accelerating discharge-to-placement timelines, hospitals can reduce average length of stay and create capacity for new admissions—without compromising on quality or safety.
- Reduce staff workload: Automation replaces tedious manual tasks such as faxing, follow-up calls, and paperwork, freeing care coordinators to focus on high-touch, high-value interactions with patients and families.
- Improve patient outcomes: With data-driven PAC matching, patients are more likely to be placed in facilities that align with their clinical needs, improving rehabilitation success rates and reducing preventable readmissions.
AI-powered referral management is not just an upgrade—it’s a strategic shift toward better care delivery and operational resilience.
If you’re committed to improving patient flow, maximizing staff efficiency, and securing financial sustainability, modernizing your referral workflow is one of the most impactful steps you can take.
Want to see a working demo? Schedule a consultation and discover how could you reduce PAC delays by 40% in just 30 days—while improving outcomes and unlocking savings.

