1. Introduction: The Challenges of Fragmented Patient Data
In the modern healthcare system, data plays a critical role in delivering effective patient care. However, despite significant advancements in healthcare technology, patient data is often fragmented across multiple systems. These silos of data exist in electronic health records (EHRs), lab reports, radiology images, and other healthcare applications, making it difficult for healthcare providers to obtain a comprehensive view of a patient’s health.
As healthcare systems become more complex and the volume of data increases, the fragmentation of patient information only exacerbates the problem. Providers may struggle to coordinate care efficiently, leading to delays, errors, and sometimes poor patient outcomes. This is where a centralized patient record system can make a significant difference—by unifying disparate data into a single, cohesive record that all providers can access, leading to better care coordination and more informed decision-making.
In this blog, we’ll explore the importance of building a centralized patient record, the challenges posed by fragmented data, and how an integrated system can benefit both healthcare providers and patients. We’ll also delve into the technologies that are helping healthcare organizations build a unified care plan and improve overall patient outcomes.
2. The Importance of Centralized Patient Records

Centralized patient records allow healthcare providers to access all relevant patient data from a single source, regardless of where or when it was collected. This unified approach to patient data is crucial for improving care quality, reducing administrative burden, and enabling faster, more accurate decision-making.
2.1 What is a Centralized Patient Record?
A centralized patient record consolidates data from various healthcare systems, including EHRs, lab results, imaging studies, prescriptions, and more, into one easily accessible platform. Rather than having this data stored in different silos, a centralized record allows healthcare providers to view a complete, up-to-date picture of a patient’s health status.
This centralized system serves as a single source of truth, ensuring that all healthcare providers have access to the same, comprehensive data. This can include:
- Medical history: Chronic conditions, past surgeries, allergies, etc.
- Lab results: Blood tests, genetic information, diagnostic studies.
- Medications: Current prescriptions, dosage, and medication history.
- Treatment plans: Current care protocols and future treatment goals.
- Patient preferences: Dietary restrictions, preferred communication methods, and personal health goals.
2.2 Why It’s Essential for Coordinated Care
When multiple healthcare providers (doctors, specialists, nurses, etc.) are involved in a patient’s care, it’s essential that everyone is on the same page. A centralized record ensures that each provider has access to the most accurate and up-to-date information, facilitating better coordination and communication between different care teams. This leads to more effective treatments, fewer mistakes, and a higher standard of care.
3. The Problems with Fragmented Data in Healthcare
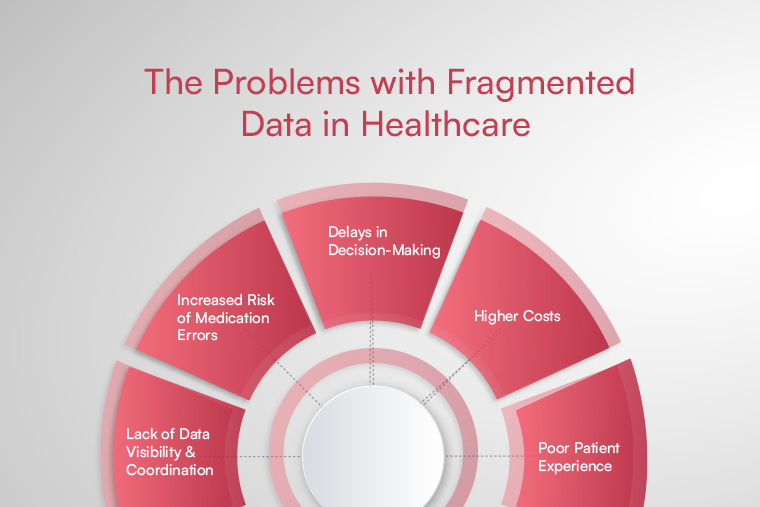
Fragmented data refers to patient information stored in multiple systems or formats, making it difficult to access, share, and analyze. This fragmentation creates significant barriers to providing optimal patient care.
3.1 Lack of Data Visibility and Coordination
When patient data is scattered across various systems, providers may not have the full picture of a patient’s health. For example, a primary care physician may not have access to recent lab results from a specialist, or a surgeon may not know about a patient’s allergic reactions documented in another system. This lack of visibility can result in fragmented care, miscommunication, and, in some cases, medical errors.
3.2 Increased Risk of Medication Errors
Fragmented patient records often mean that doctors and pharmacists do not have access to a complete list of medications a patient is taking. This can lead to medication errors—such as prescribing drugs that interact negatively with each other or duplicating medications already prescribed by other specialists.
3.3 Delays in Decision-Making
When healthcare teams have to track down missing data or rely on incomplete patient records, care decisions are delayed. This lag in decision-making can be especially detrimental in urgent care situations, where timely intervention is crucial for patient survival or recovery.
3.4 Higher Costs
The inefficiency of fragmented data often leads to increased costs for healthcare organizations. For example, hospitals may need to repeat diagnostic tests or imaging studies simply because the relevant data is not accessible from previous visits. Moreover, the time spent by administrative staff in tracking down or manually entering missing information increases operational costs.
3.5 Poor Patient Experience
Fragmented data also impacts the patient experience. Patients may have to repeat their medical history multiple times, undergo redundant tests, or experience delays in care—all because their healthcare providers don’t have access to comprehensive, unified information. This can lead to frustration, decreased trust, and lower patient satisfaction.
4. How to Build a Centralized Patient Record System
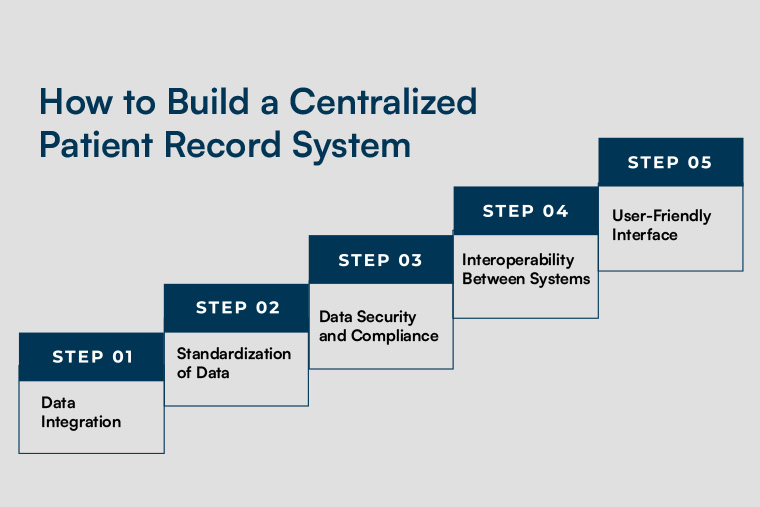
Building a centralized patient record system involves integrating various data sources into one cohesive platform. It requires careful planning, the right technology, and buy-in from all stakeholders within the healthcare system.
Step 1: Data Integration
The first step in building a centralized patient record system is to integrate data from various sources. This means connecting EHRs, lab systems, imaging systems, and other relevant tools into a unified database. Modern integration platforms can bridge the gaps between these systems and allow for seamless data sharing across departments and external healthcare providers.
Step 2: Standardization of Data
To ensure that the data is usable and accurate, standardizing the formats used across different systems is critical. Standardizing data ensures consistency in how patient information is recorded, reducing the likelihood of errors and misunderstandings. For example, using standardized medical coding systems (such as ICD-10) and consistent terminology allows data from different sources to be interpreted in the same way.
Step 3: Data Security and Compliance
Given the sensitive nature of patient data, it’s essential to ensure that the centralized system is secure and compliant with regulations like HIPAA. Hospitals must implement robust security measures such as encryption, access controls, and audit logs to protect patient information from breaches.
Step 4: Interoperability Between Systems
For a truly effective centralized patient record system, it must be interoperable with other systems used by healthcare providers. This ensures that patient data can flow smoothly across hospitals, clinics, and specialist offices, allowing for better coordination of care. FHIR (Fast Healthcare Interoperability Resources) is one of the leading standards used to enable interoperability between different healthcare systems.
Step 5: User-Friendly Interface
The system should have a user-friendly interface that allows healthcare providers to easily access, update, and share patient information. The interface should be intuitive and designed with the needs of different users (doctors, nurses, administrative staff) in mind.
5. The Benefits of a Centralized Patient Record for Healthcare Providers and Patients
A centralized patient record system offers numerous benefits for both healthcare providers and patients. These include:
5.1 Improved Patient Outcomes
With all patient data in one place, healthcare providers can make better-informed decisions, leading to more effective treatments. A centralized record helps providers spot patterns, track progress, and make proactive care decisions that prevent complications and reduce readmission rates.
5.2 Better Care Coordination
Having a single source of truth makes it easier for healthcare teams to collaborate. Whether a patient is transitioning between departments or moving from one healthcare facility to another, all care providers can access the same information, improving care coordination and reducing the risk of treatment gaps.
5.3 Streamlined Administrative Processes
A centralized record system reduces administrative overhead by eliminating the need for manual data entry, duplicate tests, and paper-based documentation. This streamlines operations, improves workflow efficiency, and frees up time for healthcare providers to focus on direct patient care.
5.4 Enhanced Patient Safety
With all data in one place, healthcare providers can easily check for allergies, drug interactions, and contraindications. This minimizes the risk of medical errors, improves medication safety, and ensures that patients receive the right treatments at the right time.
5.5 Improved Patient Experience
A centralized record improves the patient experience by reducing wait times, minimizing the need for redundant tests, and offering a more seamless care experience. Patients can also access their health information via patient portals, empowering them to take control of their own health.
6. Technologies Driving Centralized Patient Record Systems

Several technologies are at the forefront of enabling centralized patient record systems, including:
6.1 Cloud-Based Solutions
Cloud computing offers a flexible, scalable, and cost-effective solution for storing and managing patient records. Cloud-based platforms allow hospitals to securely store large amounts of data and provide access to authorized users from anywhere.
6.2 Interoperability Standards (FHIR, HL7)
Interoperability standards like FHIR (Fast Healthcare Interoperability Resources) and HL7 (Health Level 7) ensure that patient data can be shared across different healthcare systems and devices, providing a unified view of the patient’s health.
6.3 Artificial Intelligence and Machine Learning
AI and ML technologies can help analyze patient data to identify trends, predict potential health risks, and recommend personalized treatment plans. These tools can enhance the insights derived from centralized patient records, leading to better patient outcomes.
7. Conclusion: Moving Toward Clear Care Plans with Integrated Data
Building a centralized patient record system is an essential step in improving healthcare delivery. By integrating fragmented patient data into one unified platform, healthcare providers can improve care coordination, reduce medical errors, and ensure that patients receive timely and effective treatments. The use of modern technologies, such as cloud-based solutions and interoperability standards, makes it easier than ever to create a comprehensive and accurate patient record system that drives better patient outcomes.
At Cabot Technology Solutions, we specialize in creating custom healthcare solutions that integrate data across systems and enhance patient care. If you're ready to transition from fragmented data to clear care plans with a centralized patient record system, contact us today to learn more about how we can support your healthcare organization’s digital transformation.
Call to Action: How Cabot Technology Solutions Can Help You Build a Centralized Patient Record System
Are you ready to enhance patient care with a centralized patient record system? Contact Cabot Technology Solutions today to explore how we can help you build an integrated, secure, and efficient patient record solution for your healthcare facility.

