Introduction
Post‑acute care (PAC) bridges the gap between hospital discharge and full recovery. Whether patients move to a skilled nursing facility, inpatient rehab, or return home with home health support, this phase focuses on rehabilitation, monitoring, and preventing setbacks. Despite best efforts, common issues—such as post‑surgical infections, medication mix‑ups, dehydration, and falls—can slip through the cracks until they become emergencies.
Predictive analytics offers a solution: by analyzing a patient’s clinical and operational data, it flags warning signs before visible symptoms appear. Early alerts empower care teams to adjust treatment plans, schedule timely check‑ins, or arrange additional support. This proactive approach not only enhances patient safety and satisfaction but also reduces costly readmissions and conserves staff resources.
In this blog, we’ll dive into:
- What predictive analytics means in a PAC setting
- Why it’s so critical right now
- The data you need and how to integrate it
- A clear process flow (with diagram)
- Detailed use cases—from infection prevention to fall risk
- Practical steps to implement from audit to scale
- How to measure success with concrete KPIs
- Common hurdles and proven remedies
By the end, you’ll have a roadmap to leverage predictive analytics and catch complications before they escalate.
What Is Predictive Analytics?
Predictive analytics in post‑acute care is all about anticipating risks before they turn into problems. Instead of waiting for visible symptoms, it uses past and present patient data to spot subtle warning signs that might otherwise go unnoticed.
Think of it as an “early‑warning system” for your care teams:
- Alerts for Potential Complications: It can flag patients at high risk of infections, medication issues, or falls before these events happen.
- Data‑Driven Decisions: By analyzing trends in vitals, lab results, and even past admissions, it helps care teams focus on the patients who need attention most.
- Continuous Monitoring: Risk scores update in real time, meaning staff are always working with the latest information.
- Actionable Guidance: Instead of just reporting risks, it triggers specific interventions—like scheduling an urgent nursing visit or adjusting a care plan.
In short, predictive analytics turns raw patient data into clear, timely insights that help clinicians act faster, reduce complications, and improve outcomes.
Why Predictive Analytics Matters in Post‑Acute Care

- Early Intervention:
Without predictive analytics, many complications go unnoticed until vital signs worsen or patients report new symptoms. Early intervention—like adjusting antibiotics at the first sign of infection—can cut severe events by up to 50%. Timothy Lee, RN, notes that “catching sepsis before major organ dysfunction saves lives and resources.”
- Reduced Readmissions:
Readmission rates within 30 days hover around 15–20% in PAC settings. By targeting high‑risk patients for extra follow‑up—via telehealth check‑ins or home visits—organizations can reduce readmissions by 10–20%, avoiding CMS penalties.
- Cost Savings:
An avoidable readmission can cost $10,000–$15,000. Multiply that by dozens of cases per month, and you see six‑figure savings. One mid‑sized health system reported $300K in annual savings after a predictive analytics pilot.
- Improved Patient Experience:
Proactive care builds trust. Patients and families feel more secure knowing their care teams monitor warning signs continuously. Higher satisfaction scores on HCAHPS surveys translate to better hospital ratings and reimbursements.
- Staff Efficiency:
Manual chart reviews and reactive phone calls eat up nursing hours. Predictive alerts focus attention on a smaller group—high‑risk patients—freeing staff to engage in direct patient care rather than paperwork.
Data Sources and Integration
Successful predictive analytics depends on drawing from multiple, reliable data streams:
- Electronic Health Records (EHR): Core clinical data—diagnoses, medications, lab values, vitals, and narrative notes.
- Medical Devices & Wearables: Continuous feeds from remote patient monitoring (e.g., pulse oximeters, blood pressure cuffs) and in‑facility monitors.
- Pharmacy Systems: Prescription fill dates, refill adherence, and drug interaction alerts.
- Patient‑Reported Outcomes: Standardized surveys on pain, mobility, mental health, and social determinants.
- Operational Systems: Staff rosters, facility occupancy, and transfer logs to capture workload and capacity.
All inputs should flow into a centralized data lake or clinical data repository. Use interoperability standards like FHIR and HL7 to normalize data across vendors. Middleware or integration engines can map disparate data schemas into a unified format for analysis.
How It Works: Diagram Representation
.jpg)
- Patient Data Collection: Streams in structured and unstructured inputs.
- Data Integration & Normalization: Cleans, standardizes, and aggregates data.
- Predictive Modeling Engine: Runs statistical and machine learning models.
- Risk Scoring & Alerting: Assigns scores and pushes notifications.
- Clinical Intervention & Feedback: Clinicians act on alerts and feed outcomes back to the system for model refinement.
Key Use Cases
Infection Prediction
Objective: Detect early signs of sepsis, pneumonia, or urinary tract infections.
Data Points:
- Vitals: Rising temperature, heart rate spikes.
- Labs: White blood cell count, C‑reactive protein levels.
- History: Recent invasive procedures or antibiotic usage.
Action: Flag patients for immediate nursing assessment or lab draw. Early antibiotic administration can reduce ICU transfers by 30%.
Medication Error Detection
Objective: Prevent adverse drug events from interactions or incorrect dosing.
Data Points:
- Medication Lists: Current prescriptions, over‑the‑counter drugs.
- Lab Values: Kidney and liver function tests for drug clearance.
- Allergy Records: Known allergies and past reactions.
Action: Alert pharmacists to review and reconcile orders. Automated checks can cut medication errors by 40%.
Fall Risk Assessment
Objective: Identify patients at high risk of falls in facilities or at home.
Data Points:
- Mobility Scores: Gait speed, balance assessments.
- Vitals: Orthostatic blood pressure changes.
- History: Past falls, muscle weakness indicators.
Action: Trigger interventions like bed alarms, physical therapy referrals, or home safety evaluations. Programs see a 25% reduction in fall incidents.
Readmission Risk Scoring
Objective: Predict likelihood of readmission within 30 days of discharge.
Data Points:
- Clinical Complexity: Number of comorbidities, Charlson Comorbidity Index.
- Discharge Details: Length of stay, discharge disposition, home support.
- Social Determinants: Transportation access, caregiver availability.
Action: Enroll high‑risk patients in transitional care programs: scheduled home visits, medication reconciliation calls, and telehealth check‑ins—leading to a 15% drop in readmissions.
Steps to Implement Predictive Analytics
- Assess Your Data Readiness
Perform a data inventory. List all systems, data fields, and gaps.
Evaluate data quality: completeness, consistency, and timeliness.
Establish governance: assign data stewards and set up privacy/security protocols.
- Select the Right Platform
Commercial Solutions: Offer built‑in models, vendor support, and faster deployment.
In‑House Development: Provides customization and control but requires data science resources.
Compare on model accuracy, integration ease, alert delivery methods, and user interface.
- Build and Validate Models
Use retrospective data to train initial models.
Validate against a separate test set; aim for ≥80% sensitivity and specificity.
Engage clinical experts to review false positives and negatives.
- Integrate into Clinical Workflows
Embed alerts directly in the EHR or a care coordination dashboard.
Define roles: who receives alerts, how they respond, and escalation paths.
Map alerts to standardized order sets or care plans for rapid action.
- Train Your Care Team
Conduct workshops with live demos and hands‑on practice.
Provide quick‑reference guides and e‑learning modules.
Establish a help desk or “analytics champion” for ongoing support.
- Pilot and Refine
Launch in a single unit (e.g., orthopedics) to test workflows and model performance.
Collect feedback on alert relevance, timing, and usability.
Adjust risk thresholds or notification methods to minimize alert fatigue.
- Scale Across the Organization
Roll out to all PAC settings once the pilot demonstrates success.
Monitor key metrics continuously and share results in monthly performance reviews.
Schedule quarterly model retraining using newly collected data to prevent model drift.
Measuring Success
Track these key performance indicators (KPIs) to assess impact:
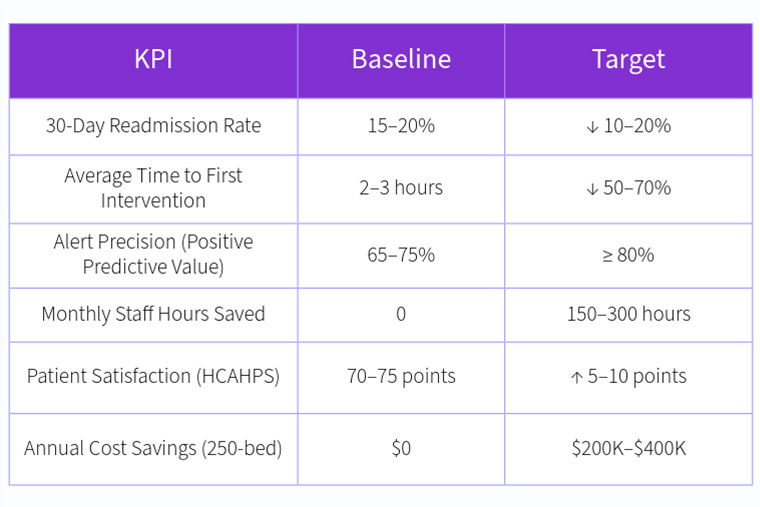
Use dashboards that update in real time, showing trends and highlighting areas needing attention. Share these metrics with executive leadership and frontline staff to maintain momentum.
Common Challenges and Solutions
- Data Silos:
Solution: Invest in a unified data platform; enforce interoperability standards (FHIR, HL7).
- Alert Fatigue:
Solution: Fine‑tune thresholds; allow clinicians to customize alert settings; bundle related alerts.
- Staff Resistance:
Solution: Involve end users early; highlight quick wins; use “analytics champions” to drive adoption.
- Model Drift:
Solution: Schedule regular retraining; monitor model performance metrics; update features as care practices evolve.
- Regulatory Compliance:
Solution: Implement strict access controls; audit trails; validate model fairness to avoid bias.
Conclusion
Predictive analytics transforms post‑acute care from a reactive to a proactive model. By continuously analyzing rich patient data, it delivers early warnings—enabling care teams to intervene before minor issues spiral into major complications. The result is smoother recoveries, fewer readmissions, happier patients, and significant cost savings.
A clear implementation path—data readiness assessment, platform selection, model validation, workflow integration, team training, and iterative scaling—ensures success. Ongoing monitoring and refinement keep your predictive models accurate and relevant.
Ready to elevate your PAC program? Schedule a call and discover how predictive analytics can help you spot complications early, optimize resource use, and deliver better patient outcomes.

