1. Introduction: The Growing Need for Post-Acute Care Innovation
Post-acute care plays a crucial role in the healthcare continuum, particularly as the aging population increases and more patients transition from hospital to long-term care facilities. However, the healthcare industry is currently grappling with challenges that hinder the efficient delivery of care in post-acute settings. One of the most pressing issues is the lack of integration between different systems used across facilities, departments, and provider networks.
For years, healthcare organizations have relied on multiple stand-alone applications for everything from electronic health records (EHRs) to patient monitoring, medication management, and appointment scheduling. While these apps serve specific purposes, they often don’t communicate with each other, creating gaps in care coordination, inefficiencies, and even safety concerns for patients.
As the demand for more comprehensive and coordinated care increases, healthcare providers must look towards interoperability as a solution to unify their systems. In this blog, we’ll explore why interoperability in post-acute care is the key to unlocking future innovation and improving patient outcomes—outperforming the trend of relying on multiple stand-alone apps.
2. The Rise of Stand-Alone Apps in Post-Acute Care

Over the last decade, the healthcare sector has seen a surge in digital solutions designed to address specific needs within post-acute care. Stand-alone apps, each targeting a distinct problem, have gained popularity for their focused features. These apps are designed to help improve certain aspects of patient care, such as:
- Medication management apps that track and remind patients of their prescriptions.
- EHR systems used to store and access patient health records.
- Telemedicine platforms that enable remote consultations with healthcare providers.
- Patient engagement apps to keep patients informed and motivated during recovery.
While these apps offer specialized functionalities, they don’t solve the larger problem of fragmentation in healthcare. When providers rely on a patchwork of individual apps that don't communicate with each other, it becomes difficult to gain a holistic view of a patient’s health and care needs. In the fast-paced world of post-acute care, this lack of interoperability can lead to costly errors, delays, and gaps in patient care.
3. Challenges with Stand-Alone Apps in Post-Acute Care
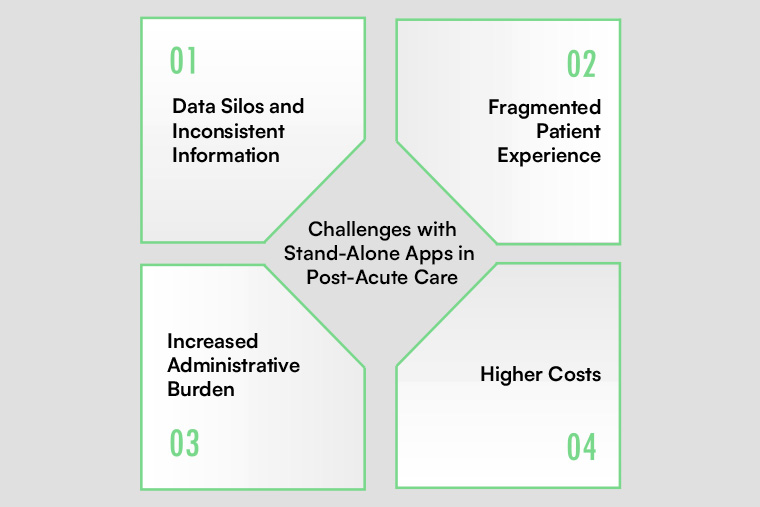
Despite their popularity, stand-alone apps present several challenges for healthcare providers and patients alike. These issues primarily arise due to the lack of communication and integration between various systems. Let’s look at some of the most significant challenges:
3.1 Data Silos and Inconsistent Information
When healthcare systems don’t integrate, valuable patient data can remain locked within separate systems. For instance, medication records in one app may not be synced with the patient's EHR or other monitoring systems. This can lead to inconsistent or incomplete information, making it difficult for care teams to provide effective care. Inconsistent data also increases the likelihood of medication errors, missed follow-up appointments, and duplication of medical tests.
3.2 Fragmented Patient Experience
Patients often struggle with managing multiple apps and platforms, each with different user interfaces, logins, and workflows. This fragmentation can result in confusion, missed appointments, and non-compliance with care plans. Patients may also become frustrated with the difficulty of accessing all their care information in one place, especially when they are transitioning from one provider to another.
3.3 Increased Administrative Burden
For care teams, managing multiple stand-alone apps can create significant administrative burden. Healthcare providers often have to manually input patient data into each system, wasting time and increasing the chances of human error. Additionally, the lack of integrated workflows means more time spent on administrative tasks, taking away from time spent on direct patient care.
3.4 Higher Costs
Maintaining multiple stand-alone systems can be costly for healthcare facilities. Each app may come with its own subscription fees, support costs, and hardware requirements. Moreover, integrating disparate systems requires significant time and resources, often resulting in a fragmented technology ecosystem that is difficult to maintain.
4. What Interoperability Brings to Post-Acute Care Innovation
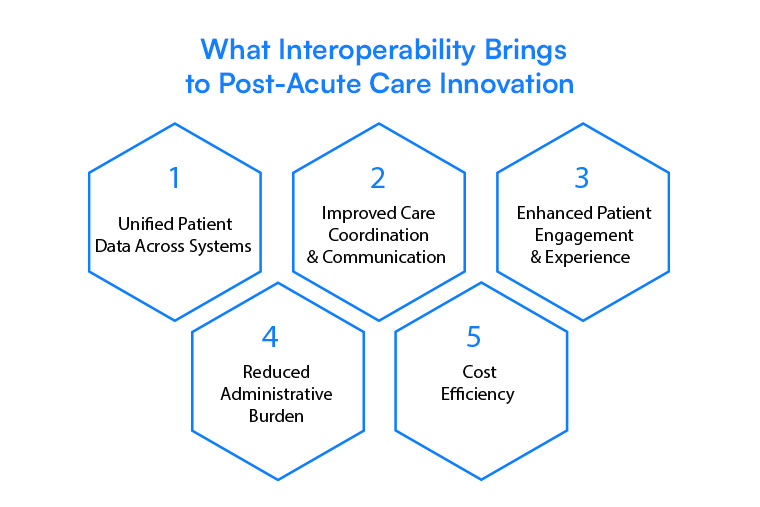
Interoperability, in its simplest form, refers to the ability of different healthcare systems and technologies to communicate and share data seamlessly. When applied to post-acute care, interoperability offers numerous advantages over the use of stand-alone apps:
4.1 Unified Patient Data Across Systems
Interoperability allows for the integration of multiple systems, ensuring that patient data flows seamlessly across various platforms. This eliminates data silos and ensures that healthcare providers have access to the full spectrum of a patient’s health history, including medications, test results, treatment plans, and more. With this comprehensive view, care teams can make better-informed decisions and provide more effective, coordinated care.
4.2 Improved Care Coordination and Communication
With interoperable systems, communication between different healthcare providers—such as SNFs, hospitals, home health agencies, and physicians—becomes streamlined. When everyone is on the same page, patients receive better coordinated care, reducing the risk of complications or miscommunication. Providers can collaborate more efficiently on treatment plans, improving patient outcomes while also saving time.
4.3 Enhanced Patient Engagement and Experience
Patients benefit from interoperability as well. By having all their health data integrated into a single platform, they can access their information at any time and from any location. This consolidated view of their care allows them to better manage their health, follow through with appointments, and track their progress. It also reduces the burden of managing multiple apps, leading to a more seamless and patient-centered experience.
4.4 Reduced Administrative Burden
Interoperability reduces the administrative burden by eliminating the need for healthcare workers to manually input patient data into multiple systems. Automated data sharing and syncing save time and reduce errors, allowing providers to focus more on delivering care and less on administrative tasks.
4.5 Cost Efficiency
By consolidating various systems into one interoperable network, healthcare organizations can reduce the costs associated with maintaining multiple stand-alone apps. With fewer systems to manage, organizations can invest in more powerful, integrated solutions that improve care quality and lower long-term operational expenses.
5. How Interoperability is Shaping the Future of Healthcare

Interoperability is no longer just a buzzword—it’s rapidly becoming a critical component of healthcare innovation. The future of healthcare is moving toward a unified ecosystem where data flows freely and securely between systems, creating a connected experience for patients and providers alike.
5.1 The Shift to Value-Based Care
The shift from fee-for-service to value-based care requires improved care coordination and efficient use of resources. Interoperability enables better communication across the care continuum, leading to more effective treatment plans and healthier patients, which are essential for value-based care success.
5.2 Emerging Technologies and Interoperability
New technologies, such as Artificial Intelligence (AI), Machine Learning (ML), and Blockchain, are expected to play a major role in driving healthcare interoperability. These technologies can analyze vast amounts of patient data to provide insights that help clinicians make better decisions. As healthcare systems evolve, interoperable networks will enable these technologies to function optimally, unlocking new levels of innovation and precision medicine.
5.3 Government and Industry Push for Interoperability
Governments and regulatory bodies are increasingly pushing for healthcare interoperability. In the U.S., the 21st Century Cures Act mandates that healthcare organizations adopt interoperable systems to improve patient care and data access. These regulations are paving the way for a future where patient data can easily be shared across facilities, promoting transparency, patient choice, and better overall healthcare delivery.
6. Conclusion: Moving Towards a Unified, Efficient Post-Acute Care System
The future of post-acute care innovation hinges on the ability to create a unified, interoperable healthcare ecosystem. Stand-alone apps, while useful in specific scenarios, ultimately fall short when it comes to providing the comprehensive, coordinated care that patients need during transitions from hospital to home or skilled nursing facilities. Interoperability offers the solution, enabling better data sharing, streamlined workflows, improved patient outcomes, and lower costs.
As healthcare evolves, interoperability will play an increasingly important role in shaping the future of care. Healthcare providers must begin embracing integrated solutions that break down silos and enable seamless communication across the entire care continuum.
At Cabot Technology Solutions, we specialize in developing interoperable solutions that help healthcare organizations bridge the gaps between systems, improve care coordination, and drive innovation. With our expertise in cloud-based solutions, EHR integration, and healthcare analytics, we can help your organization move toward a future where interoperability is the standard, not the exception.
Ready to move beyond stand-alone apps and embrace a unified, interoperable healthcare system? Contact Cabot Technology Solutions today to learn how we can help your facility adopt interoperable solutions that improve care coordination, streamline operations, and enhance patient outcomes.

