Introduction – When “No Vacancy” Isn’t a Choice
Walk into any hospital discharge office today and you’ll hear the same refrain: “We called every skilled-nursing facility in town—no one can take the patient.” It isn’t that beds have vanished; it’s that caregivers to staff those beds are in short supply, and traditional fax-and-phone admissions can’t keep pace with demand. The outcome is a painful ripple: hospitals board patients longer, families scramble for placement, and nursing-home operators lose revenue they can’t afford to forfeit.
Yet behind the headlines lies an encouraging truth. The core of the problem is operational, not clinical, and software purpose-built for post-acute referrals can remove many of the artificial walls that keep doors shut. This article unpacks why facilities are limiting admissions and shows how modern, cloud-based referral hubs give them the confidence—and capacity—to say “yes” again.
The New Reality of Capacity Caps
Staffing Shortages that Won’t Quit
Even after wage bumps and signing bonuses, positions for certified nursing assistants and licensed nurses remain stubbornly unfilled. Administrators describe a relentless churn: new hires arrive, only to burn out under mandatory overtime or leave for hospitals offering flexible schedules. Facilities that once greeted every referral with a cheerful “Send them over” now triage inquiries against the painful question, Do we have enough hands on the floor for tonight’s shift?
Shrinking Licensed Capacity
Faced with chronic understaffing, many operators have closed wings, converted double rooms into singles, or blocked off entire hallways for safety. The building still stands, but inspected capacity quietly drops. In rural areas, one wing closure can force patients to travel hours from home for rehab, straining families and hospital discharge teams alike.
Hospital Bottlenecks and Public Quality Scores
When skilled-nursing beds go dark, the logjam shifts upstream. Hospital case managers must call a longer list of facilities and repeat the same hand-offs. Every extra day a patient waits on a medical-surgical floor costs the hospital dearly and risks downstream penalties for delayed transitions. Meanwhile, consumer-facing star-ratings now highlight “timely and safe transitions,” so facilities that decline or delay too often find themselves sliding down comparison charts. The reputational impact is immediate and punishing.
In short, staffing may light the spark, but the tinder that keeps the fire roaring is an admissions process rooted in paper, faxes, and manually re-keyed spreadsheets.
The Hidden Costs of Manual Intake

Manual admissions rarely appear on a balance sheet, yet they erode margins in countless ways:
- Lagging response times – Hospitals often blast the same referral to a dozen facilities and accept the first positive reply. If your intake nurse must sort through illegible fax pages and chase laboratory results by phone, you lose precious minutes—sometimes hours—during which the bed sits empty and someone else claims the resident.
- Staff exhaustion and overtime – Intake work seldom fits neatly inside daytime hours. Nurses field late-night calls, fax logs pile up over the weekend, and administrative staff spend Mondays frantically processing a backlog. The overtime costs are obvious; the turnover that follows is costlier still.
- Vacant beds and payer-mix drift – Every delay risks a high-margin referral slipping away, while lower-acuity or less profitable residents take their place. Over time the census declines, even though rooms technically remain “open.”
- Denied authorizations and payer friction – Hand-written forms invite errors: a wrong policy number here, a missing diagnosis code there. Each mistake lengthens the authorization cycle or pushes the resident into a less favorable reimbursement category.
- Blind-spot analytics – Paper logs don’t deliver dashboards. Without data on which hospital sends which payer mix, marketing campaigns become guesswork and regional growth stalls.
Collectively, these hidden leaks drain resources faster than any single line item—yet they are precisely the leaks cloud referral platforms are designed to seal.
How Cloud-Based Referral Hubs Work
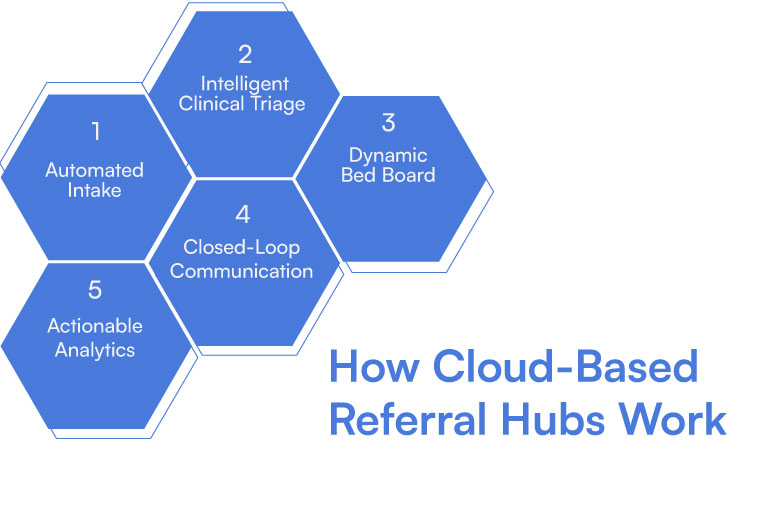
Post-acute care referral software replaces scattered faxes and siloed inboxes with a single, secure web console that anyone on the admissions team can open from a workstation, tablet, or even a phone. Under the hood, five pillars transform chaos into clarity:
- Automated Intake
The platform ingests referrals arriving via fax, Direct secure messaging, HL7, FHIR, or simple email attachments. Optical character recognition and natural-language processing extract demographics, insurance data, therapy minutes, and clinical notes, so intake staff see a clean, structured profile without re-keying information.
- Intelligent Clinical Triage
Built-in rules and AI models flag isolation requirements, complex wounds, dialysis needs, or bariatric equipment at a glance. Instead of paging a nurse to sift through pages manually, the system surfaces key risk factors instantly, helping staff render safe, confident decisions.
- Dynamic Bed Board
Integration with the facility’s clinical and scheduling systems means the platform knows which beds are staffed and truly available—not just licensed on paper. When a referral arrives, available rooms appear in real time, making the fateful “Can we take this resident?” conversation simple rather than speculative.
- Closed-Loop Communication
Once staff click “accept,” the decision posts straight back to the hospital’s EMR, and the discharge nurse receives immediate confirmation. Phone-tag evaporates. If the case must be declined, the hospital gains rapid clarity and can reroute their patient without delay.
- Actionable Analytics
Dashboards track response times, acceptance rates, payer mix, and average length of stay by referral source. Leadership sees trends before they become crises and can focus marketing where margins are best.
Why Cloud Matters
A cloud deployment brings several intrinsic advantages:
- Elastic capacity handles seasonal spikes without servers to patch.
- Security certifications and audit trails satisfy regulators and risk officers.
- Browser-based access means admissions aren’t tethered to a particular desk, easing after-hours coverage.
- Upgrades roll out automatically, so new analytics or compliance measures arrive without an IT project.
The Soft-But-Serious Return on Investment
Operators often ask, “Will this pay for itself?” Without quoting exact figures you’ll find in Cabot’s whitepaper, consider the qualitative shifts that follow implementation:
- Faster turn-arounds keep high-acuity referrals from leaking to competitors and ensure weekend discharges aren’t lost to Monday delays.
- Reduced overtime lowers burnout and turnover, nudging staffing stability upward without additional hiring.
- Improved payer mix emerges as analytics reveal which hospitals send residents whose reimbursement aligns with the facility’s strategy. Admissions teams can then prioritize or court those partners.
- Shorter authorization cycles mean fewer billing headaches and stronger cash flow.
- Richer data equips leadership to make evidence-based expansion or consolidation decisions rather than reacting to anecdote.
Many operators find that the intangible benefits—staff satisfaction, stronger hospital relationships, and greater reputational standing—are every bit as valuable as the hard revenue lift.
Five Practical Steps to Adoption
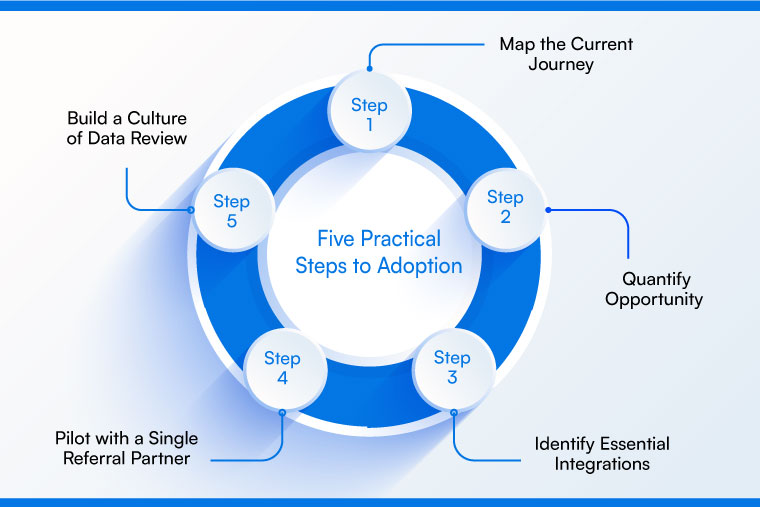
Transitioning from a fax-driven process to a cloud hub is less daunting than it appears when tackled methodically:
Step 1: Map the Current Journey
Follow a referral from the moment it hits the fax tray to the instant a resident wheels through your doors. Every hand-off holds a potential stall. Seeing the flow end-to-end clarifies where technology will have the greatest impact.
Step 2: Quantify Opportunity
Even if you leave specific numbers to finance, capture narratives: How often are beds empty while staff shuffle paperwork? How many promising cases slipped away because the hospital “never heard back”? Stories anchor the business case to lived reality.
Step 3: Identify Essential Integrations
At a minimum, connect your clinical record, e-fax service, and insurance verification. Add scheduling or staffing modules as comfort grows. Modular adoption prevents scope creep and accelerates go-live.
Step 4: Pilot with a Single Referral Partner
Select a hospital already inclined to collaborate. A month-long pilot surfaces real-world gains and fine-tunes workflows before you scale across the network.
Step 5: Build a Culture of Data Review
Technology alone cannot sustain momentum. Schedule brief weekly stand-ups to review dashboards: Which hospitals convert fastest? Which declines were preventable? Shared, transparent metrics transform intake from reactive firefighting into proactive performance management.
Conclusion – Turning “No” Back into “Yes”
Nursing-home leaders cannot conjure nurses out of thin air, but they can remove needless friction from the path every referral travels. Cloud-based post-acute care referral software clears that path, shrinking decision times from a sluggish crawl to a confident, real-time stride. The payoff reaches well beyond fuller beds: staff regain control of their shifts, hospitals regain trust in their community partners, and families feel the relief of quicker placement.
In a market where the difference between thriving and merely surviving often hangs on operational agility, digitizing admissions is no longer a nice-to-have advantage—it is essential infrastructure. Facilities that act now will not only weather today’s staffing storms but also position themselves as preferred destinations for tomorrow’s discharge planners.
Ready to Go Deeper?
Download Cabot’s free PDF, “The AI Intake Playbook,” for a detailed breakdown of outcomes, implementation timelines, and real-world case studies. Or schedule a call to understand how Cabot helped other PAC clients.

